Having lost 3 of 6 counselors in GCASA'a Albion office I have been helping out doing evaluations. I have done 10 in the last 2 weeks and it is an enlightening experience. I want to capture and share some of my experience.
1. The paperwork is overwhelming. A great deal of it is unnecessary and amounts to checking boxes and collecting data and filling in boxes that have nothing to do with the client's primary concerns nor does it help in establishing therapeutic rapport or obtaining good outcomes. The paperwork has been promulgated in response to regulatory requirements and reimbursement mechanisms not good clinical practice. Regulatory have no good means of measuring good treatment and good outcomes and so they rely on compliance with paperwork completion as a proxy for good treatment. This is a false assumption, and a dangerous way of evaluating good care. Staff are constantly harassed to treat the medical record not the client and the acknowledgement and recognition of good programs depends on compliance with paperwork requirements not the interaction and service provision to clients.
2. As stated in #1, good treatment is determined by correct completion and compliance of paperwork not client satisfaction or good treatment outcomes. Unfortunately, this has perverted the system of care and the primary customer of service has become the regulator and the payer not the client.
3. It has been impressed on me once again that self destructive behavior should not be equated with criminal behavior. Most of the clients I evaluated were sent by the criminal justice system or other governmental bodies such as the Department of Social Services, the Department of Motor Vehicles, Probation, the courts, etc. The health care system for substance abuse disorders has been captured by government to coerce behaviors which government has determined is in its own best interest and not necessarily in the individual's. What Michel Foucault calls "governmentality" increasingly deprives individuals from their freedom. There is a fine line between whether agencies like GCASA are health care agencies whose mission is to help individuals improve their health or coercive agents of social control. It looks to me like 75% of GCASA's services are designed to exert social control and the client's right to self determination is marginalized if respected at all.
I have further observations and thoughts which I will share in future posts.
GCASA is an acronym for the Genesee/Orleans Council on Alcoholism and Substance Abuse, Inc. whose administrative offices are in Batavia, NY. The articles and opinions are those of the authors and not necessarily the offical positions of GCASA. New content is added daily so bookmark this blog and/or subscribe.
Thursday, October 22, 2009
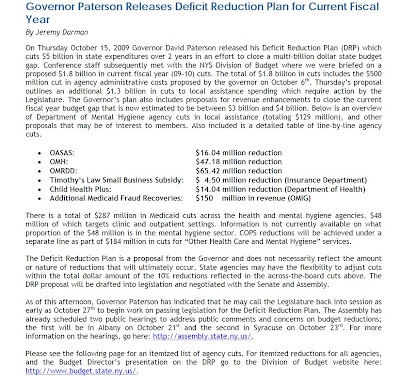
Governor proposes 16 million in cuts to OASAS as part of Deficit Reduction Plan
Tuesday, October 20, 2009
17th Annual Batavia Halloween Parade
Monday, October 19, 2009
Back in the trenches
We've lost 3 of our 6 counselors in our Albion office for a variety of reasons. The requests for service have escalated and last week we had 25 requests for intakes.
There is no more money. No increase in our county and state funding. No increase in our reimbursements, not in 10 years.
Yes, you've read that right. Not in a decade.
Now the governor is cutting the state budget and how it will affect substance abuse services isn't clear, but it isn't pretty.
So, I'm the kind of executive director who rolls up his shirt sleeves and helps out. Last week I did 8 intakes.
I'm almost 64 years old. I've been in the field 41 years, and I'm back where I started, providing direct services where they are needed most, on the front lines.
I wonder if the commissioner of OASAS can provide the kind of leadership I provide?
No, she is not a substance abuse professional. She wouldn't have a clue.
I wonder if the regional office staff could do what I'm doing?
No, they re making sure the Ts are crossed and the Is are dotted. They are counting beans as if the patient with DTs cares.
At the end of the day, somebody has to do the work - actually see patients. The people who actually do the work, are the lowest paid, the most harassed by the bureaucrats, the ones criminalized by the Medicaid fraud units because the treatment plans didn't get signed in the designated time frames.
As I leave my administrative desk and actually see patients again, I am reminded that something is terribly wrong with our service delivery systems. We have inverted the system so that the most highly paid, the most highly recognized, the most highly rewarded are the ones furthest away from the actual work.
I am enjoying seeing patients, but the budgets and regulatory paperwork is getting behind so I will leave the patients to suffer waiting for care while Albany makes its paperwork demands, and silly meetings have to be attended, and we pretend that the policy makers and the regulators have the really important work to do.
This week I will do both, see patients and work on my paperwork, but I do so with a renewed awareness about what the work really means and the value it really has, something that too many leaders have never known, or forgotten, or maneuvered to get promoted away from to where the real money is and there is alot less stress and pressure, and in some ways, responsibility.
I am taking care of patients again not worrying about corporate compliance. I have been doing God's work, not the work for soulless bureaucrats.
There is no more money. No increase in our county and state funding. No increase in our reimbursements, not in 10 years.
Yes, you've read that right. Not in a decade.
Now the governor is cutting the state budget and how it will affect substance abuse services isn't clear, but it isn't pretty.
So, I'm the kind of executive director who rolls up his shirt sleeves and helps out. Last week I did 8 intakes.
I'm almost 64 years old. I've been in the field 41 years, and I'm back where I started, providing direct services where they are needed most, on the front lines.
I wonder if the commissioner of OASAS can provide the kind of leadership I provide?
No, she is not a substance abuse professional. She wouldn't have a clue.
I wonder if the regional office staff could do what I'm doing?
No, they re making sure the Ts are crossed and the Is are dotted. They are counting beans as if the patient with DTs cares.
At the end of the day, somebody has to do the work - actually see patients. The people who actually do the work, are the lowest paid, the most harassed by the bureaucrats, the ones criminalized by the Medicaid fraud units because the treatment plans didn't get signed in the designated time frames.
As I leave my administrative desk and actually see patients again, I am reminded that something is terribly wrong with our service delivery systems. We have inverted the system so that the most highly paid, the most highly recognized, the most highly rewarded are the ones furthest away from the actual work.
I am enjoying seeing patients, but the budgets and regulatory paperwork is getting behind so I will leave the patients to suffer waiting for care while Albany makes its paperwork demands, and silly meetings have to be attended, and we pretend that the policy makers and the regulators have the really important work to do.
This week I will do both, see patients and work on my paperwork, but I do so with a renewed awareness about what the work really means and the value it really has, something that too many leaders have never known, or forgotten, or maneuvered to get promoted away from to where the real money is and there is alot less stress and pressure, and in some ways, responsibility.
I am taking care of patients again not worrying about corporate compliance. I have been doing God's work, not the work for soulless bureaucrats.
Monday, October 12, 2009
Indigenous Peoples Day
Today is Indigenous Peoples Day or Columbus Day if you prefer.
Indigenous people have suffered from substance abuse more than most whether is is the result of genetic predispositions, from genocide, from cultural disposssosion or a little of both.
Please stand in solidarity with indigenous peoples this day and be a resource, if possible in their recovery.
Indigenous people have suffered from substance abuse more than most whether is is the result of genetic predispositions, from genocide, from cultural disposssosion or a little of both.
Please stand in solidarity with indigenous peoples this day and be a resource, if possible in their recovery.
Thursday, October 8, 2009
A Guide for Substance Abuse Services for Primary Care Physicians
A Guide For Substance Abuse Services for Primary Care Physicians. To access click here.
Monday, October 5, 2009
Cocaine laced with veterinary anti-parasite drug
SAMHSA (Substance Abuse and Mental Health Services Administration)released an alert on 09/21/09 that cocaine in some regions has been found to be laced with a veterinary anti-parasite drug which is very toxic to humans. You can read the alert by clicking here.
Thursday, October 1, 2009
Death from Opioid Overdose is a big concern
Those of us who work in the Substance Abuse field all know of patients who have died from Opioid overdoses. Every time this happens we are reminded once again that substance abuse can be a terminal illness.
OASAS (New York State Office of Alcoholism and Substance Abuse) and DOH (New York State Department of Health) have issued a Health Advisory entitled "Interventions To Prevent Opioid Overdose". You can access it by clicking here.
OASAS (New York State Office of Alcoholism and Substance Abuse) and DOH (New York State Department of Health) have issued a Health Advisory entitled "Interventions To Prevent Opioid Overdose". You can access it by clicking here.
Helping female vets in New York State
From the NYS Conference of Mental Hygiene Directors Newsletter for September 25, 2009.
NYS Office of Alcoholism and Substance Abuse Services (OASAS) Commissioner Karen M. Carpenter-Palumbo announced that Samaritan Village will break ground on a 25-bed facility designed specifically to meet the rehabilitative needs of women veterans, the first of its kind in New York. Samaritan Village has 11 facilities throughout the state, providing substance abuse treatment, homeless services, senior services, and veterans' services.
"Nearly 17 percent of the armed forces are women," said Commissioner Carpenter-Palumbo. "There are 66,000 women veterans in New York State alone, many of whom have experienced the physical and emotional traumas of combat in addition to sexual harassment or assault, which we know when left untreated, often lead to substance use disorders. Women veterans return home expected to resume their role as wife, mother, professional, or family caregiver, but if they are suffering, quietly or not, from post traumatic stress disorder, substance use disorders, mental health issues, or the self-imposed guilt or shame of sexual assault, then we all lose: the individual, the family and the community.” She added, "Samaritan Village is committed to the veterans it serves, and I congratulate them on leading the charge with a unique women's program that is truly first in the nation."
This specialized women's veterans program is made possible through $5 million in funding from the OASAS, and is the result of an RFP released by the state to build 100 residential treatment beds for veterans throughout New York.
In 2007, seven percent of the near 14,000 veterans admitted to the state's treatment system were women — that's almost 1,000 female veterans in need of gender-specific, individualized care. The multifaceted experiences of women in the military generate a need for varied types of treatment upon their return. Vital to their overall health, well-being, long-term recovery, and reintegration into society is treatment provided in a safe and reassuring environment. The U.S. Department of Veterans Affairs now has staff within every region who serves as a Women Veteran Program Manager to help women veterans connect to expanded health care benefits offered through VA Healthcare. VA Hospitals now provide maternity care, gynecological care, osteoporosis screening and treatment, mental health, as well other health care services. To find a local Women Veteran Program Manager in your region, call 1-800-877-222- VETS (8387).
NYS Office of Alcoholism and Substance Abuse Services (OASAS) Commissioner Karen M. Carpenter-Palumbo announced that Samaritan Village will break ground on a 25-bed facility designed specifically to meet the rehabilitative needs of women veterans, the first of its kind in New York. Samaritan Village has 11 facilities throughout the state, providing substance abuse treatment, homeless services, senior services, and veterans' services.
"Nearly 17 percent of the armed forces are women," said Commissioner Carpenter-Palumbo. "There are 66,000 women veterans in New York State alone, many of whom have experienced the physical and emotional traumas of combat in addition to sexual harassment or assault, which we know when left untreated, often lead to substance use disorders. Women veterans return home expected to resume their role as wife, mother, professional, or family caregiver, but if they are suffering, quietly or not, from post traumatic stress disorder, substance use disorders, mental health issues, or the self-imposed guilt or shame of sexual assault, then we all lose: the individual, the family and the community.” She added, "Samaritan Village is committed to the veterans it serves, and I congratulate them on leading the charge with a unique women's program that is truly first in the nation."
This specialized women's veterans program is made possible through $5 million in funding from the OASAS, and is the result of an RFP released by the state to build 100 residential treatment beds for veterans throughout New York.
In 2007, seven percent of the near 14,000 veterans admitted to the state's treatment system were women — that's almost 1,000 female veterans in need of gender-specific, individualized care. The multifaceted experiences of women in the military generate a need for varied types of treatment upon their return. Vital to their overall health, well-being, long-term recovery, and reintegration into society is treatment provided in a safe and reassuring environment. The U.S. Department of Veterans Affairs now has staff within every region who serves as a Women Veteran Program Manager to help women veterans connect to expanded health care benefits offered through VA Healthcare. VA Hospitals now provide maternity care, gynecological care, osteoporosis screening and treatment, mental health, as well other health care services. To find a local Women Veteran Program Manager in your region, call 1-800-877-222- VETS (8387).
Subscribe to:
Comments (Atom)